Abstract
Background: Hereditary hemolytic anemias (HHAs) are a heterogeneous group of rare disorders, with clinical presentation varying from asymptomatic to severe anemia. HHAs are characterized by red cell destruction, at times caused by enzyme deficiencies such as pyruvate kinase (PK) deficiency (due to mutations in the PKLR gene). Given the rarity of PK deficiency and the overlap of clinical presentation with other HHAs, routine diagnostic techniques can be inconclusive in many patients (pts). Next generation sequencing (NGS) may allow more sensitive and specific diagnosis of HHAs, including PK deficiency. A no-cost diagnostic program for pts with suspected HHA has been available since 2018 (ARUP® 2018-2020, AnemiaID/PerkinElmer® 2020-present) to provide diagnosis using an NGS panel of anemia-associated genes. Here, we describe the results from pts tested using this program and who were identified to carry ≥1 reportable variant(s) in the PKLR gene.
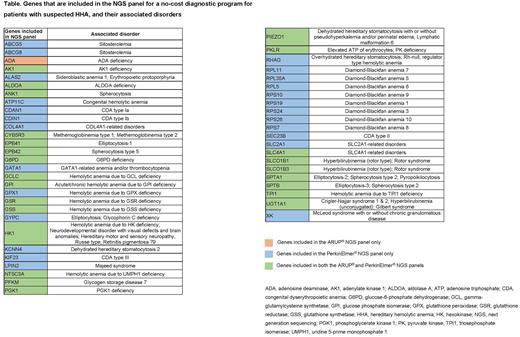
Methods: The NGS panel used in this analysis includes ~50 genes (Table) encoding cytoskeletal proteins and enzymes relating to HHA, including enzymopathies such as PK deficiency and similar disorders with overlapping clinical features, and covers the complete coding region, splice site junctions, and, where appropriate, deep intronic or regulatory regions. Targeted gene capture and library construction for NGS were performed using a Whole Blood and Saliva kit (PerkinElmer®) and sequenced on Illumina® NGS systems. Samples were sequenced using 150 bp paired-end sequencing at target average coverage of 80×. NGS output data were summarized descriptively for all pts.
Results: Samples from 1007 pts were run from July 2018 to May 2022. Of these samples, 74 (7%) were identified with ≥1 reportable PKLR variant and included in this analysis; 23/74 (31%) samples were heterozygous, 33/74 (45%) were heterozygous for 2 PKLR variants, and 18/74 (24%) were homozygous for PKLR variants. There were 127 PKLR variants reported, 91 (72%) of which were classified as likely pathogenic (LP)/pathogenic (P) and 36 (28%) were variants of uncertain significance (VUS). In addition, 2 pts had large homozygous deletions. The majority of variants (80%) were missense mutations. Based on available clinical data from 58 pts, there were 30 pts for whom diagnostic or likely diagnostic result was established in the PKLR gene. This included 21 pts homozygous or compound heterozygous for LP/P sequence variants, 1 homozygous for deletion, 6 with 2 LP/P PKLR variants of unknown phase, and 2 compound heterozygous for LP/P and a VUS. Inconclusive, but possible diagnostic PKLR findings were identified in 7 pts: 4 homozygous or compound heterozygous for PKLR VUS variants, 3 with LP/P and a VUS with phase unknown. Others were inconclusive because only 1 PKLR variant was identified (n=14) or the diagnosis was identified in other genes (n=7).
PK enzyme levels ranged from <1.1 to 8.5 U/g hemoglobin (Hb). Most (21/37; 57%) pts with available PK enzyme levels had <2.0 U/g Hb. In addition, 3 pts had a molecular diagnosis in the PKLR gene and normal PK enzyme levels (>5.5 U/g Hb), 2 of whom had received a transfusion in the prior 2 weeks. Adult (≥18 years [yrs]) and pediatric pts (<18 yrs) were distributed evenly in the cohort (53% and 47%, respectively); 30/74 (41%) were older than 30 yrs at testing, of whom 18/30 (60%) were older than 50 yrs.
Conclusions: NGS is an effective platform for the diagnosis of PK deficiency. Most pathogenic variants identified were small sequence variants, but large deletions in PKLR are not uncommon and should be part of the NGS panel. In addition, over 40% of the pts tested were >30 yrs of age, some of whom were without a previous diagnosis, emphasizing the complexity of a PK deficiency diagnosis in pts with lifelong anemia. NGS, through this no-cost diagnostic testing program, may help to make a diagnosis in situations where PK enzyme levels may be inconclusive or potentially confounded (pts receiving frequent transfusions). With the recent advances in drug development and the approval of a new medicine for pts with PK deficiency, improved diagnosis may increase awareness of the disease and allow for appropriate treatment and counselling for these patients.
Disclosures
McGee:Agios Pharmaceuticals, Inc.: Current Employment, Current holder of stock options in a privately-held company.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal